An American man claims he contracted a superbug in his penis from a bidet — and it left him urinating blood for days.
Molson Hart took to X to share his experience of what he initially thought was a cold which later turned out to be an E.coli infection in his genitals.
Describing his experience in graphic detail, he claimed doctors told him the infection — which comes from faeces — was resistant to standard antibiotics.
Mr Hart, who runs an educational toy company, pinned the infection on a bidet splashing e.coli contaminated water onto his penis.
However, medics and other social media users were sceptical and suggested a different, more risqué, way E.coli could have entered Mr Hart’s urethra.

Molson Hart, pictured, took to X to share his experience of what he initially thought was a cold which later turned out to be an E. coli infection in his genitals that left him urinating blood

As to how E.coli ended up in his urethra to begin with, Mr Hart, who runs an educational toy company, pinned the infection on his bidet
Writing on X, Mr Hart said: ‘When you use a bidet it shoots water at your butthole and E. coli is in healthy people.
‘Well I shot water into my butt which then ended up getting shot into my penis. That’s the best explanation I can come up with.’
Within hours the post has amassed more than 32 million views and gathered 1,700 comments.
One critic, summing up the views of many on the thread, suggested: ‘All this is an elaborate excuse to hide the fact that you had a one night stand.’
E.coli infections that cause UTIs are commonly contracted after sex.
Another simply wrote: ‘Dude did a*** and is covering up cheating on his wife.’
In an attempt to explain his theory further, Mr Hart posted an anatomical diagram of how the bidet could have sprayed dirty water from his anus into his penis.
However, users were quick to point out he had added to the length of the penis in the drawing in order to make this possible, which either meant Mr Hart was very well endowed or perhaps stretching the truth.

To explain himself further Mr Hart posted an anatomical diagram of how the bidet could have sprayed dirty water from his anus into his penis

Studies have suggested E. coli accounts for 90 per cent of urinary tract infections
In a follow-up post, Mr Hart insisted he was not a ‘gay man on the down low’, and even theorised hamburger meat from a McDonald’s hamburger, with the chain recently experiencing a E. coli outbreak, could also be to blame.
‘Did some of their E.coli infected grinder meat fall into my penis?,’ he wrote.
Urologists commenting on the post however, were skeptical that a bidet was to blame for Mr Hart’s experience.
One, called Dario, highlighted how E.coli was one of the most common causes of urinary tract infections (UTIs) in general, and it could have multiple causes beyond some sort of toilet bowl trickshot.
‘E.coli is one of the most common UTI pathogens and in males, it can occur from urinary obstruction, residual urine and foreign bodies in the urinary tract (like stones).
‘You didn’t get it from a bidet,’ he wrote.
He added: ‘The fact that yours was resistant to an antibiotic is concerning, as is your presentation with hematuria (the medical term for blood in urine).’
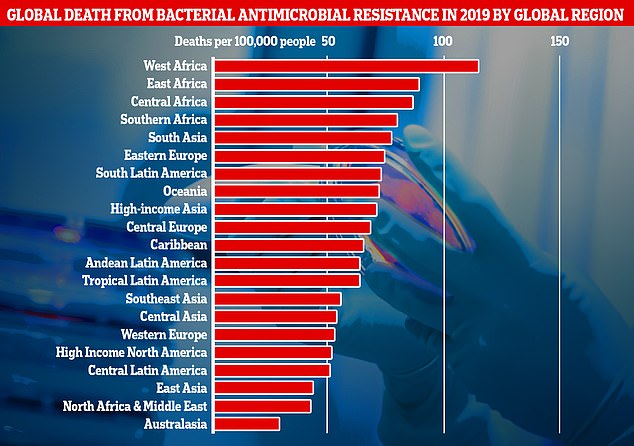
This graph shows the combined direct and associated deaths from antibiotic-resistant bacteria per global region measured in the new research. Africa and South Asia had the greatest number of deaths per 100,000 people, however Western European countries like, the UK, still recorded a significantly high number of fatalities

Figures showed a recent sharp increase in the number of prescriptions for antibiotics following years of decline. According to the UKHSA, 58,224 people in England had an antibiotic-resistant infection in 2022, up four per cent on 2021
Mr Hart said he first felt unwell a few days before his diagnosis but dismissed as a cold the rest of his family had recently come down with.
However, when it started to burn when he urinated he sought medical help and was diagnosed with a standard UTI.
But things took a dramatic turn a day later when Mr Hart saw he was passing coagulated blood and he rushed himself to the emergency room.
‘Ohhhh that really hurts. Is that a booger? Oh no it’s coagulated blood,’ he said.
Urine tests then revealed he had an antibiotic resistant strain of the bug.
Studies have suggested E. coli accounts for 90 per cent of UTIs and kidney stones or some other obstruction are a potential cause.
Penetrative sex, both heterosexual and homosexual, is also another, as well as poor hygiene and conditions that make it difficult for the bladder to fully empty such as an enlarged prostate.
Some health conditions, such as diabetes or having a weakened immune system, can make it more likely for bacteria to be able to infect the urethra rather than the body resolving it without any symptoms occurring.
The fact Mr Hart’s infection was of an antibiotic resistant variant of E. coli is unusual as most cases are easily resolved with standard medications.
However, experts across the globe are concerned about the rise of such variants, dubbed ‘superbugs’, though the technical term for the phenomenon is ‘antimicrobial resistance’ (AMR).
AMR, in a variety of pathogens, already kills an estimated 1.2million people globally each year, more than HIV or malaria, and contributes to the deaths of 5million more.
In Britain specifically AMR is thought kill almost 8,000 Brits a year with many more suffering long term health consequences from having been infected.
The World HEalth Organization predicts the global direct death toll from AMR will grow to 10million per year by 2050.
Over and inappropriate use of drugs like antibiotics is one of the driving factors behind bugs developing AMR.
This includes people taking antibiotics when they don’t need to but also giving them to farm animals on an industrial scale in an attempt to pre-emptively stop infections and boost profits.
Such agricultural use allows massive amounts to leak into the environment, where wild pathogens can develop a resistance.
Experts have warned that if AMR becomes increasingly widespread it could lead to routine surgeries, as well as treatments that lower the immune system like chemo and organ transplants, becoming far riskier with potentially deadly consequences.
One of few ways AMR can potentially be combatted is the development of new classes of antibiotics that pathogens have not yet had the chance to adapt to.
However, no such breakthroughs have been made since the 80s.
One barrier to developing new drugs is cost. Industry estimates suggest the cost of developing one new antibiotic is £1 billion, far below the estimated revenue of selling one of roughly £35 million a year.
Revenue is predicted to be so low because health chiefs will only deploy these drugs as a last resort, in a bid to stop, or slow, pathogens developing a new resistance to them and taking AMR back to square one.
Different funding models have been suggested to fix this, like a subscription model that pays companies for access for superbug beating drugs on an annual basis regardless of use, but these have yet to bear fruit.










