Bacteria can get “hangry” — irritable as a result of hunger — just like humans, a study has determined. A lack of nutrients, microbiologists found, causes some bacterial cells to release harmful toxins into our bodies that can make us sick. While the present study focussed only on one bacteria, should the findings hold true for other species, such could open up new treatments for infection.
The study was undertaken by microbiologist Professor Adam Rosenthal of the University of North Carolina at Chapel Hill and colleagues from Harvard and Princeton Universities, as well as the Dutch pet food firm Danisco Animal Nutrition.
Prof. Rosenthal said: “Bacteria behave much more differently than we traditionally thought.
“Even when we study a community of bacteria that are all genetically identical, they don’t all act the same way. We wanted to find out why.”
The team used a recently discovered method of analysis — “probe-based bacterial sequencing” — to read the RNA molecules of thousands of individual bacteria.
The team sequenced the transcriptome of three species. These included Escherichia coli, the model organism Bacillus subtilis, and Clostridium perfringens.
The latter bacterial species is commonly found in nature and is a leading cause of food poisoning.
The researchers determined that genetically identical cells within a single bacterial community have different functions.
Some bacteria, the researchers found, behave in a more docile fashion, while others produce toxins that make us feel ill.
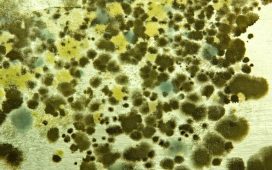
Among C. perfringens, the team identified a bacterial subpopulation that produces and releases a toxin known as “netB”.
However, this only occurs in the absence of acetate, a short-chain fatty acid that is highly prevalent in the gut.
READ MORE: Bacterial ‘suicide squads’ find tumours and alert body’s immune system
Based on the finding that nutrients play a significant role in bacterial toxicity, Prof. Rosenthal said that he now wonders if there might be particular factors found in the environment that “turn on” toxin production in other bacterial pathogens beyond C. perfringens.
If so, it is possible that introducing nutrients to bacteria could provide a new way to treat bacterial infections from both humans and animals alike.
In fact, C. perfringens is known to infect hens — being both highly infectious and fatal for the birds — and as the poultry industry moves away from the use of antibiotics, new defences are needed against the disease.
Accordingly, the new study suggests a potential new way for farmers to reduce pathogenic bacteria among their flocks without recourse to antibiotics.
With their initial study complete, the researchers are now continuing their research into the behaviour of these complex bacterial communities.
Prof. Rosenthal is also looking to apply the findings of their study to tackle the problem of antibiotic tolerance.
Tolerance limits the effectiveness of antibiotics, but the mechanisms which control it are not well understood.
The full findings of the study were published in the journal Nature Microbiology.