Pancreatic cancer is one of the most deadly forms of the disease.
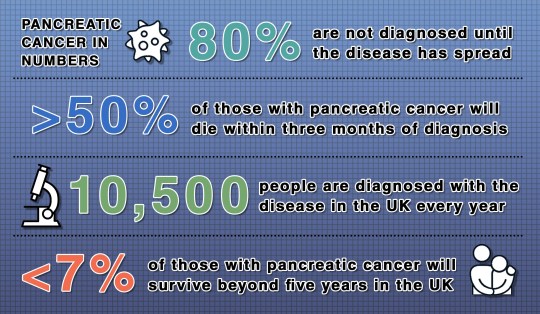
More than 10,000 people in the UK are diagnosed with pancreatic cancer every year. Of these, 80% will not be diagnosed until the cancer has spread, and only 30% will be given active treatment to combat it.
Less than seven per cent of those with pancreatic cancer will survive more than five years.
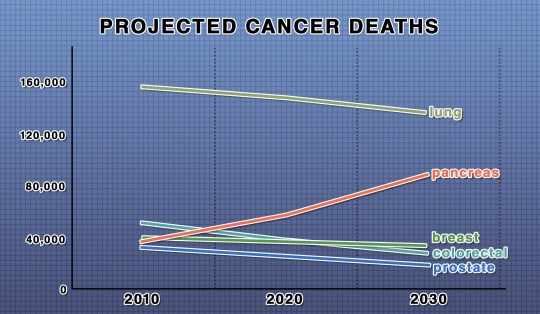
Those shocking statistics have changed very little since the 1970s, during which time survival rates for other cancers have soared.
Between the 1970s and 2010, the 10-year survival rate for bowel cancer improved from 22% to 57%, and the one-year breast cancer survival rate is now around 97%.
Why pancreatic cancer is so difficult to treat lies in its many symptoms.
What are the symptoms of pancreatic cancer?
Symptoms of the pancreatic cancer include indigestion, tummy or back pain, changes to your poo, unexplained weight loss or loss of appetite, or jaundice – yellow skin or eyes, or itchy skin.
Other less common symptoms include recently diagnosed diabetes, nausea, blood clots and fatigue.
Why is pancreatic cancer so hard to treat?
The wide range and vague nature of its symptoms mean it is very hard to pinpoint pancreatic cancer as the source of the problems.
Dr Chris Macdonald, head of research at Pancreatic Cancer UK, says: ‘Other types of cancer have “alarm symptoms”, something very specific that people know they should see their GP about.
‘The example I always use is breast cancer – if you spot a lump [you see your doctor].
‘But pancreatic cancer symptoms are myriad, and they should rightly be attributed to other conditions before you get to cancer.
‘However, that means people are bounced around a lot between seeing their GP and getting a diagnosis, for as much as up to two years in 91% of cases.’
As a result of the difficulties diagnosing pancreatic cancer, 80% of people are diagnosed late – at stage 3 or 4 – by which time the disease has often metastasized, or spread.
‘The vast majority of people that we treat for pancreatic cancer are actually being treated for a systemic disease, meaning it has spread out of the primary tumour and moved elsewhere in the body, such as the lungs or liver,’ says Dr Macdonald.
How is pancreatic cancer treated?
‘It’s a sad fact that 70% of people diagnosed with pancreatic cancer don’t go on to have any active treatment,’ says Dr Macdonald.
Due to the late stage of the disease, by the time many are diagnosed, the only treatment available is palliative care – focused on providing pain relief and easing the symptoms rather than tackling the cause.
The only known cure for pancreatic cancer is surgery, which involves not only removing the pancreas but also a large portion of the gastrointestinal tract – digestive system – around the organ.
‘If people are diagnosed early enough you can operate, but it’s incredibly complex and not a small undertaking,’ says Dr Macdonald.
‘The surgery is called a Whipple’s procedure, and takes many hours of highly trained surgical time to essentially remove the middle component of your gastrointestinal tract, so that itself comes with its own risks.’
What is the pancreas?
The pancreas is a gland in the digestive system
It has two main functions – to help digest food by producing enzymes, and maintain blood sugar by producing the hormones insulin and glucagon
It is about 20cm long and sits between the stomach and the spine
Diabetes is caused when the pancreas does not produce enough, or any, insulin – or the body’s cells do not respond to the insulin produced
In addition to major surgery, by removing the pancreas, the operation requires lifelong medication to replace the organ’s function – which includes producing insulin to regulate blood sugar levels.
Patients may also be given chemotherapy, used to help slow the disease rather than cure it.
‘One of the consequences of late diagnosis is there are limited treatment options, and so they’ve often been adapted from other cancers,’ says Dr Macdonald.
‘And that transfer of chemotherapy to people with pancreatic cancer from other cancer types isn’t very effective because those patients are inherently already very ill.
‘To go back to breast cancer – you can have a lump in your breast but also be running marathons.
‘But with pancreatic cancer people are severely ill, then they’re provided with a potent cocktail of poison developed for other cancer types where people are more resilient, and the combination can often be too much for them.’
What are the risk factors?
Many of the potential risk factors for pancreatic cancer are unclear, but evidence suggests that age, smoking and being overweight or obese can increase the risk, as can a family history of the disease, pancreatitis and diabetes.
Other factors that some evidence has shown increase the risk include alcohol, red and processed meat and gallstones.
What next for pancreatic cancer?
Unlike many other cancers, survival rates for the disease have not increased significantly in recent decades in the UK.
Pancreatic Cancer UK has recently launched a campaign calling on the next government to prioritise the disease after what it calls ‘decades of neglect’.
‘Research fundamentally saves lives,’ says Dr Macdonald. ‘We need to make true breakthroughs and transformational changes towards survival.
‘We really need to have the research and a long-term commitment towards research investment that allows us to get the breakthroughs that we’ve seen in other cancer types and other conditions on the back of strong continuous funding.
‘So what we’re asking for is, whoever wins the next election, that they prioritise pancreatic cancer as an investment of research. We’re asking for at least £35 million a year for a sustained period, over 10 or 20 years.’
MORE : Housing migrants on sites like Bibby costs £46,000,000 more than hotels
MORE : What would happen if King Charles abdicated the throne?
MORE : A mystery infection is spreading across Japan and no one knows why
Get your need-to-know
latest news, feel-good stories, analysis and more
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.